
Despite working in healthcare for many years, the day I went into hospital as a patient, I changed. I felt vulnerable, other people had my fate in their hands. I felt scared, what was going to happen to me, was I going to be ok? I felt inferior, I didn’t know what to fully expect or what I could ask about and I just let other people decided for me. Afterwards, I felt frustrated and embarrassed. Why did I feel like this when I manage NHS staff, have worked in the NHS for many years and have a really good understanding of how things work? If I feel like this, how do people with no insight feel?
We sometimes forget the emotions a hospital stay can cause patients. We can be working in healthcare, rushing around meeting demands, filling out forms, chasing down actions or going from task to task without fully realising what the patient is going through. It can be easily overlooked with the constant flow of patients coming and going. You might think these feelings are expected when going into hospital, but, they shouldn’t be. Imagine, a patient not knowing what is happening to them – would we allow that to happen to us as a person in our day to day life? Why should we when we become a “patient?” Imagine, as a patient, you are really worried about something that is hurting you or causing problems, but you are too scared to speak up or dismiss it as you don’t want to bother staff. This could be something significant that stops you from coming to harm but you don’t voice it. Imagine, you know something isn’t right, but no one is listening. You feel powerless and anxious but sit quietly. Who do you go to next? How do you find the confidence to speak up?
About a year ago, I embarked on a process for looking at how we communicate with our patients. I started to read ward leaflets and the top 5 things that stood out were:
- Length. After a while, I got bored and did’t finish some. There was just too much information to get through and my attention was wavering. If I was not engaging with them, I wondered if patients actually read them all and thought “that’s what I need to do/can do/should do.” Paragraph after paragraph with words for the sake of words. Some of it wasn’t relevant to empowering or informing the patient. Some didn’t give them advice on what to do or expect.
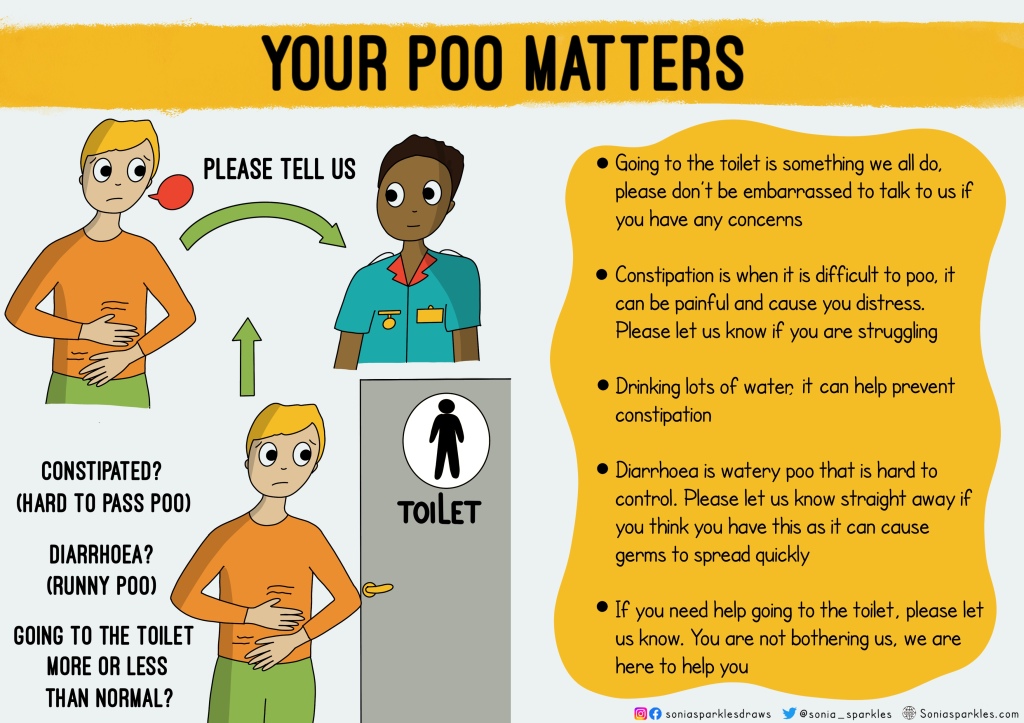
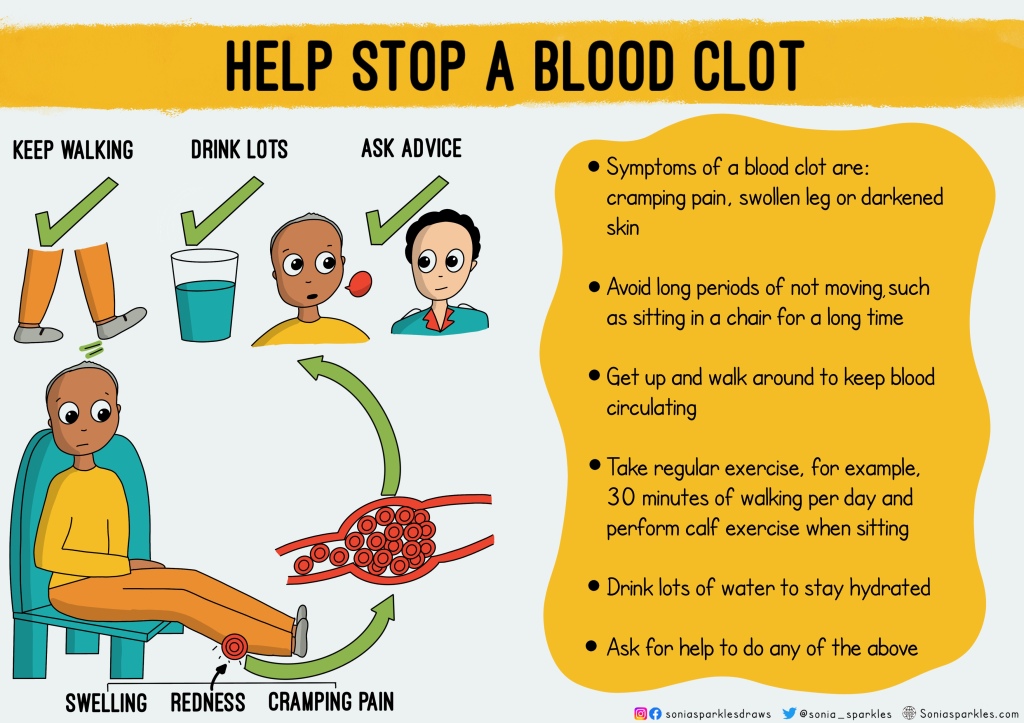
- Language. Some of the leaflets had complex words that could be difficult for others to understand. Some had phrases that were probably not common outside the healthcare context. One example is “opening your bowels;” not everyone understands what this means and it is a medicalised way of saying “having a poo.” We shouldn’t be too politically correct of phrases that don’t hold meaning to most people. Another example is “Deep Vein Thrombosis – DVT” most people won’t know what this means, whilst they would have eventually understood it the further they read the leaflet, it would have been much simpler to just use “blood clot.”
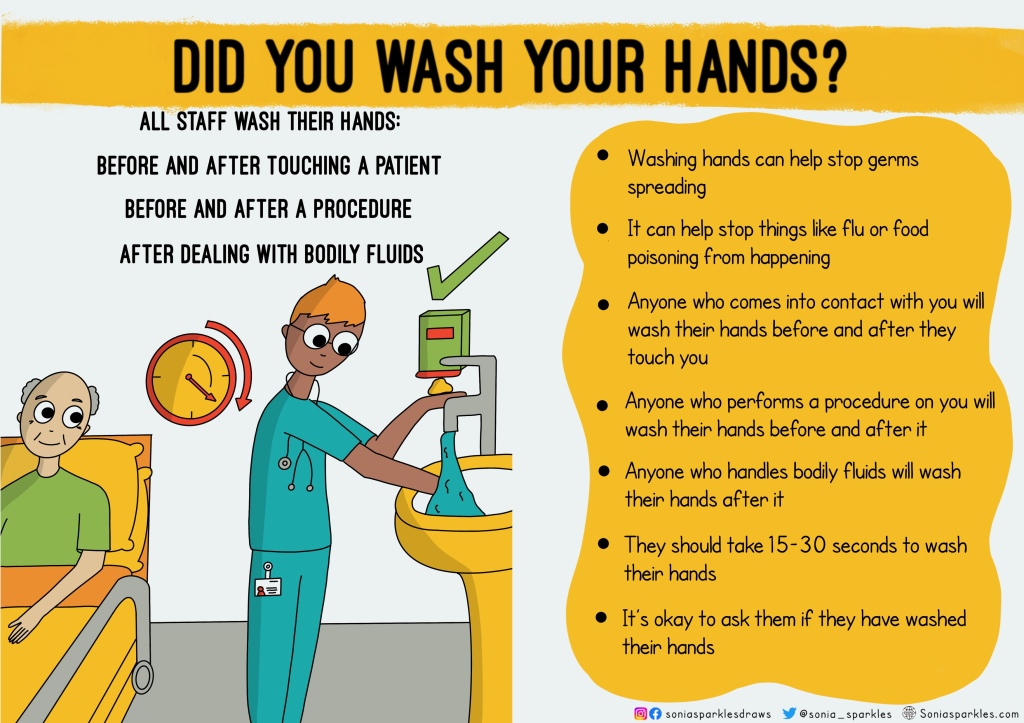
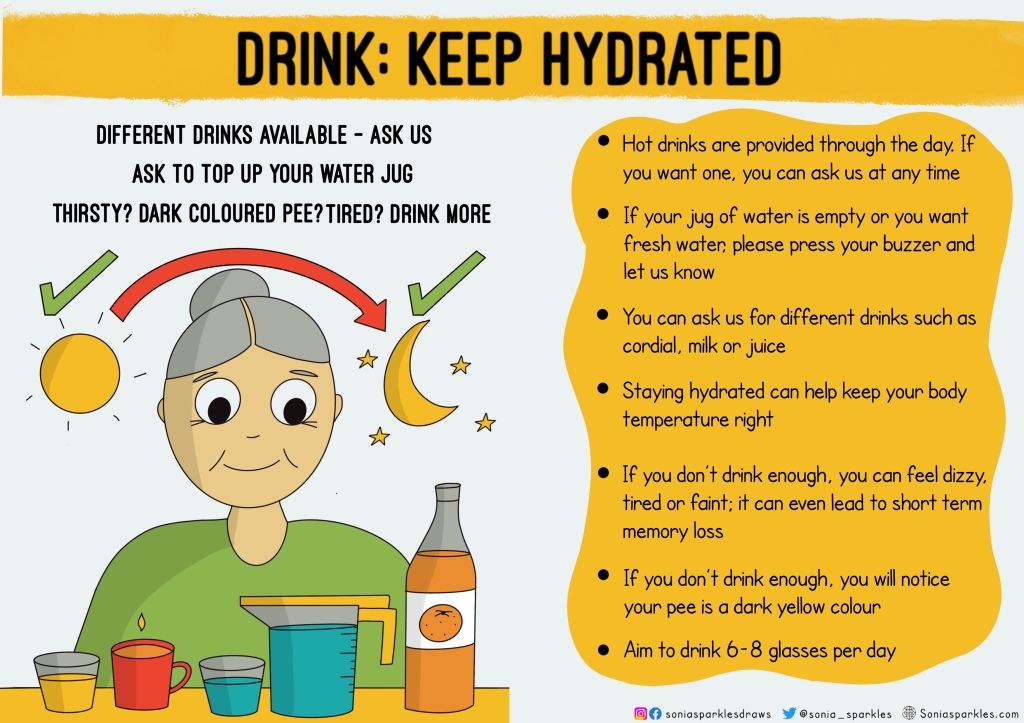
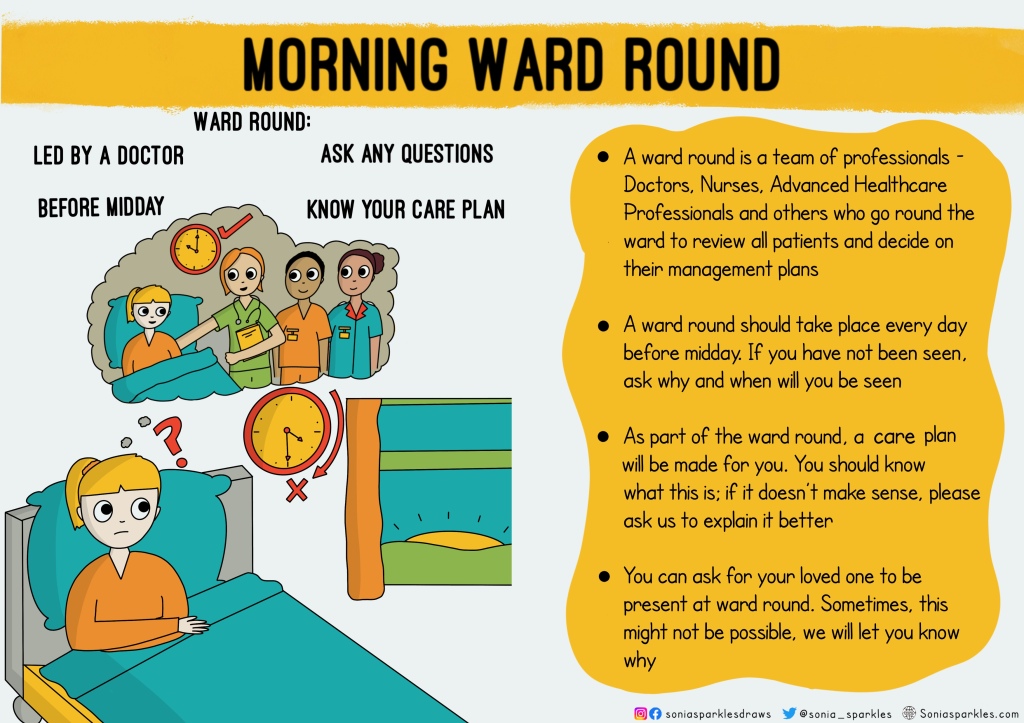
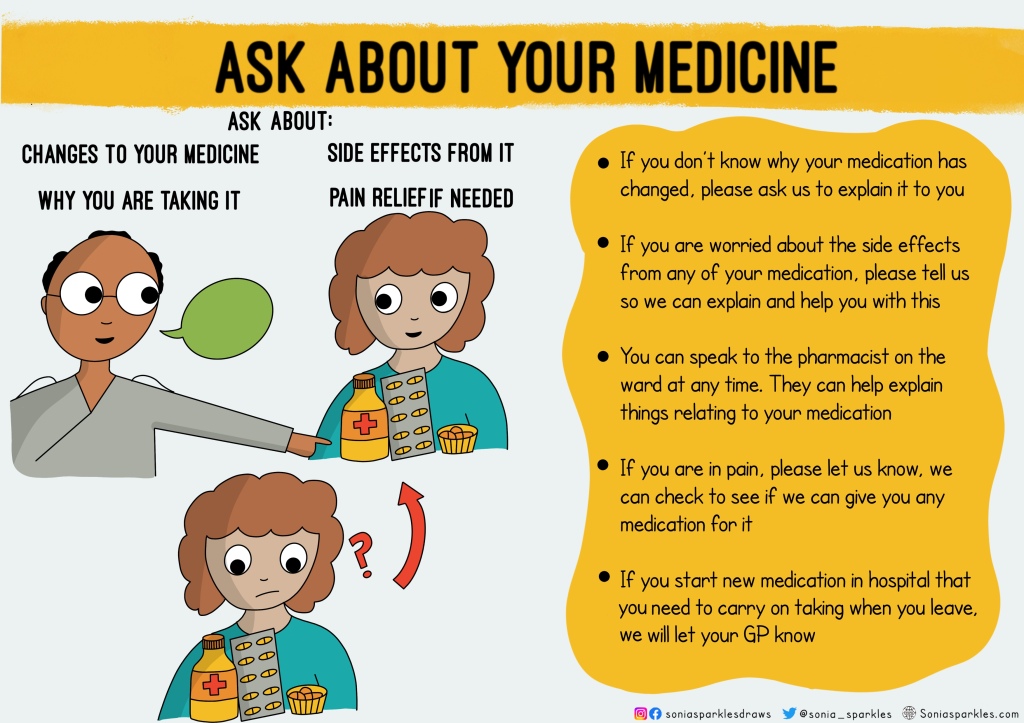
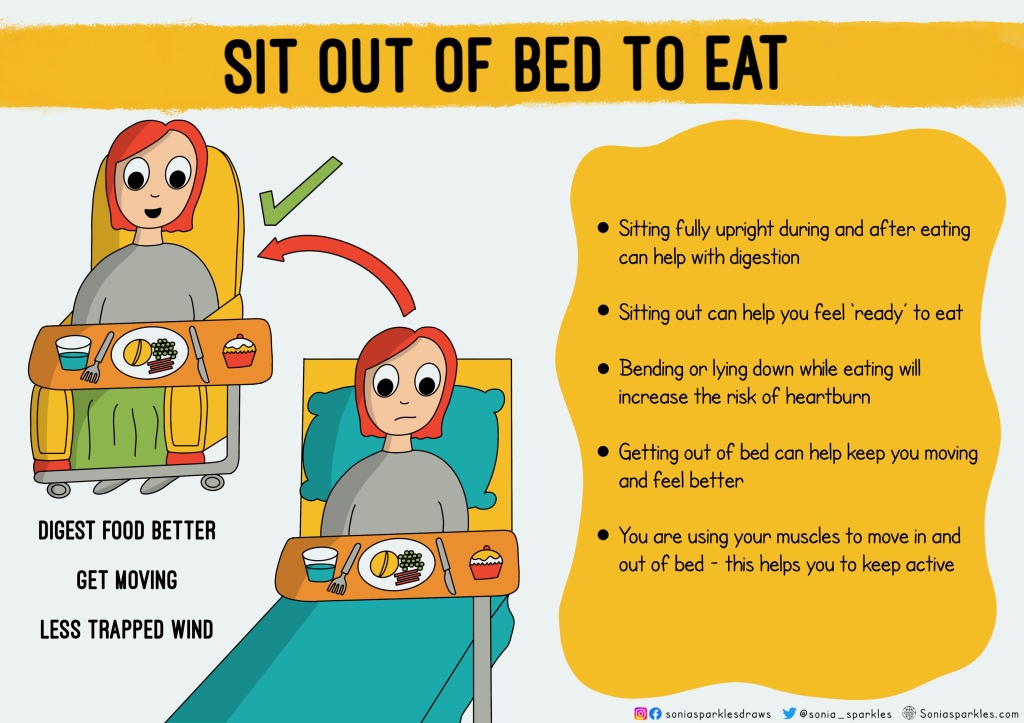
- Images. Some leaflets had no meaningful images/photos/pictures to aid the reader whilst they read the leaflet. Images are needed to help connect meaning to words and can be useful for patients who have cognitive impairment or language barriers. A simple picture can help keep the reader’s attention on the information, help them to understand what is being said and act as a reminder for them throughout their hospital stay
- Perspective. As I read the leaflets, I kept thinking, who are they written for? Why are they written? Some felt as though they were there to “protect” the ward from risk; some to inform the patient of what the ward expects and others to tell the patient about the logistics on the ward. All valid information, but, I found myself questioning where’s the patient empowerment? Where’s the encouragement to get them asking questions? Where’s the qualitative aspects of their hospital stay like sleep, drinks and getting dressed?
- Emotion. I’ve touched on this, but I will expand. I found most leaflets lacked any sense of emotion. Now remember, this leaflet could be given to someone who is scared, vulnerable and feeling inferior. Information is power, making them feel welcome gives confidence and letting them know it’s ok to ask will help them to speak up. Most leaflets were “matter of fact” and whilst some did say “speak to us if you have concerns” it felt very corporate.
So having read the leaflets, I questioned myself too. As someone who works in the NHS, I realised I too can get sucked into the corporate, risk stratified, jargon loving healthcare we work in. It’s not a criticism, it’s an opportunity to reframe and think about our communication methods. I know all patient information goes through internal patient communication committees for approval, yet, some still lacks the 5 points listed above. That’s because whatever way we slice it, the leaflet is written by a healthcare professional with their clinical/departmental perspective in mind. Rarely do we throw the rule book away and say let’s ask the patient first, what do you want to know? how do they feel? what empowers them? Information is more than just informing, it has to go beyond that to inspire patients to be able to DO SOMETHING when they need to. Leaflets need to offer encouragement, reassurance and direction to the reader. It’s not a passive bit of paper.
With this in mind, I started to think of all the information I had read and what is it that patients actually need to know about? what is it that they need to look out for? what should they challenge/ what should they ask? what should they expect? All of these things can transform their care, experience, how long they are in hospital and ultimately save lives. Yes save lives. Many times, I have read serious incident reports or cases of harm/complaints where the patient of family members say they weren’t listened to, weren’t aware of what to expect or how they feel regretful they didn’t raise that concern they had at the time. You read reports where patients didn’t want to “bother” staff or felt like a nuisance if they raised a point. We can do something about this and it starts with consistent empowering information to all patients that covers the points discussed above
A year down the line, I have drawn a series of 23 posters as a starting point to get people thinking about how we communicate with our patients in a simple, visual and empowering way. It was no easy task and yes I used people in my life who have been in hospital (with no hospital experience) to ask them how they felt and what they wanted to know
If you want to use any of them you can get them here
A summary of the posters:
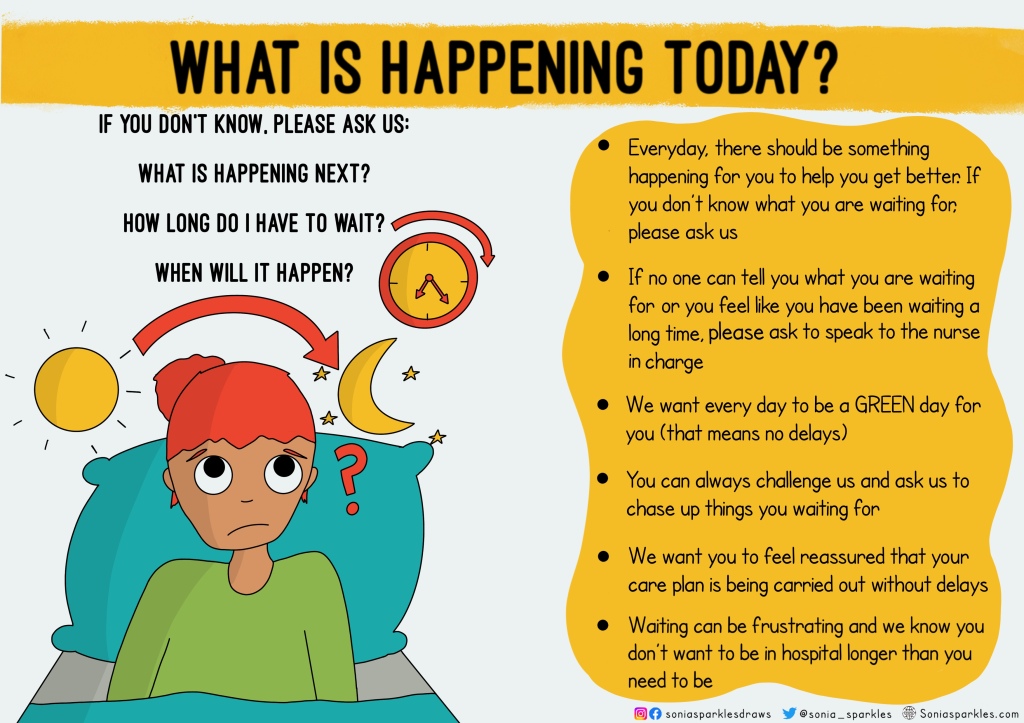
What is happening today? Encouraging patients to hold us to account for what they are waiting for. Time is precious to them. It can be frustrating stuck on a ward waiting for something to happen. It can add to unnecessary days wasted in hospital.
Name and job role. We take it for granted that patients know what our role is and what we offer them. It can be confusing for them seeing many different professionals, they don’t know who they should turn to about different questions they might have.
A name is our connection. “Hello my name is…what name would you like to be called?” is much more active and engaging. Knowing a name means they know who said what and who to call upon if needed.

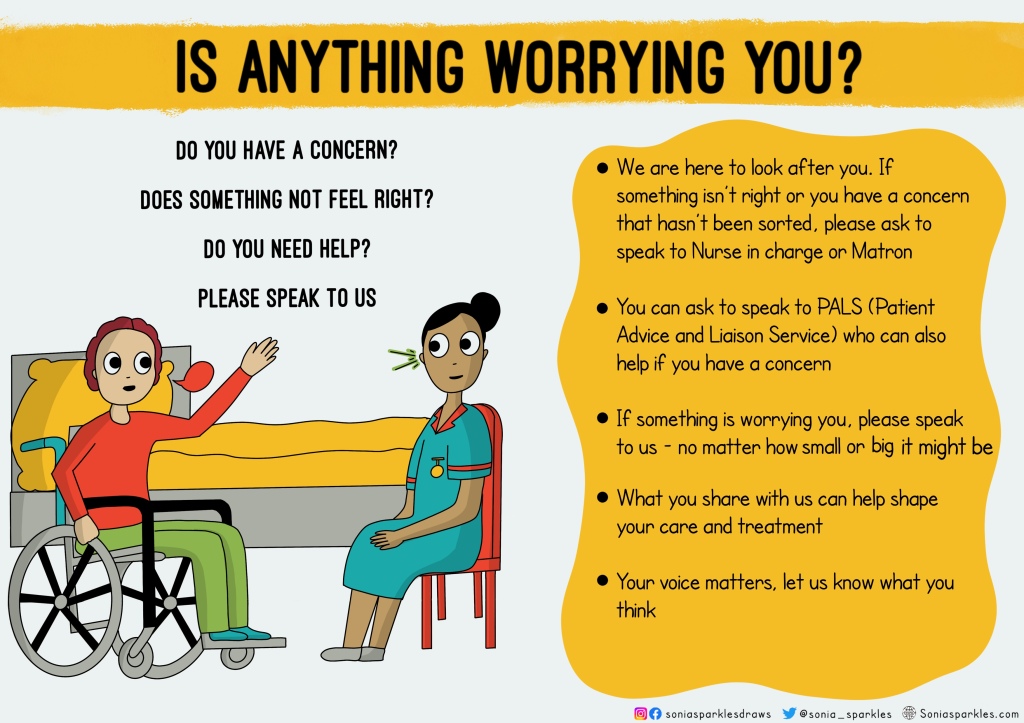
Is anything worrying you? One of the most important points all communication material should cover is encouraging patients to speak up. This could mean a concern, worry, idea or experience. Many leaflets reference PALS and complaints – such a strong word that could deter people from raising something they wouldn’t class as a “complaint.” Knowing who to speak to can help ensure they are listened to. Patients who might feel unheard or scared to challenge and need to know who else they can go to. It can literally save a life.
Helping you get home. Behind the scenes, there are lots of staff promoting and chasing up SAFER standards; yet not many patients know what it is and what to expect. We have managers and flow team chasing these up, but what if, the person we are doing it for (patient) also did this and held us to account? They are not passive participants in this.

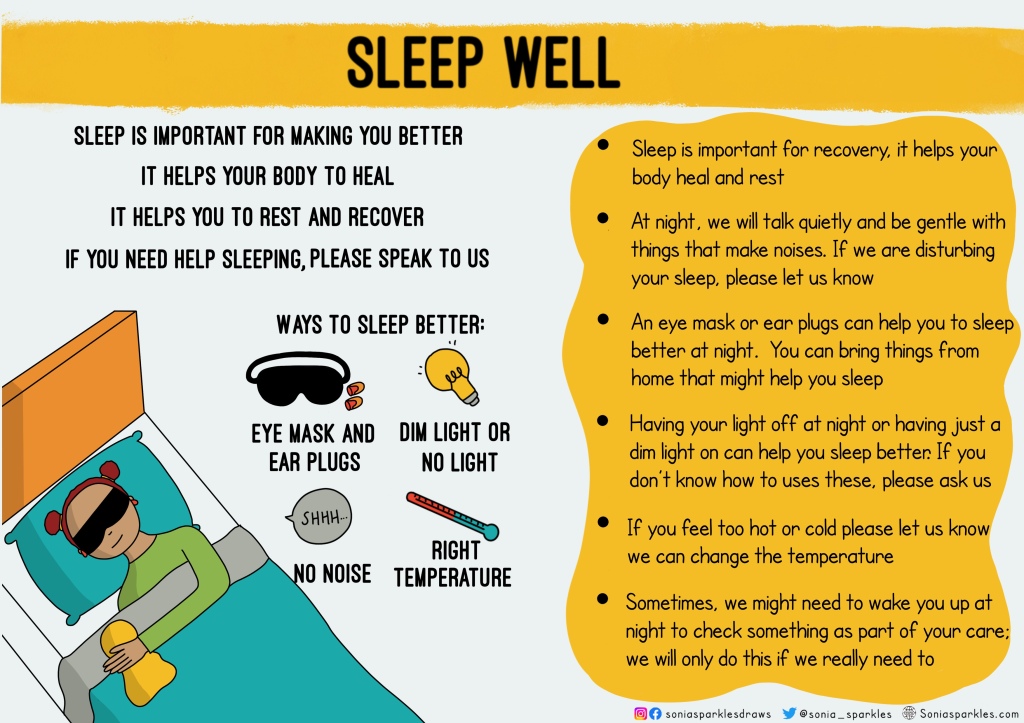
Sleep well. Good quality sleep can help patients get better – physically and mentally. Do they know they can challenge us if we are disturbing them at night e.g. loud talking, loud phone ringing, loud bin lid. We should empower them to feel comfortable telling us
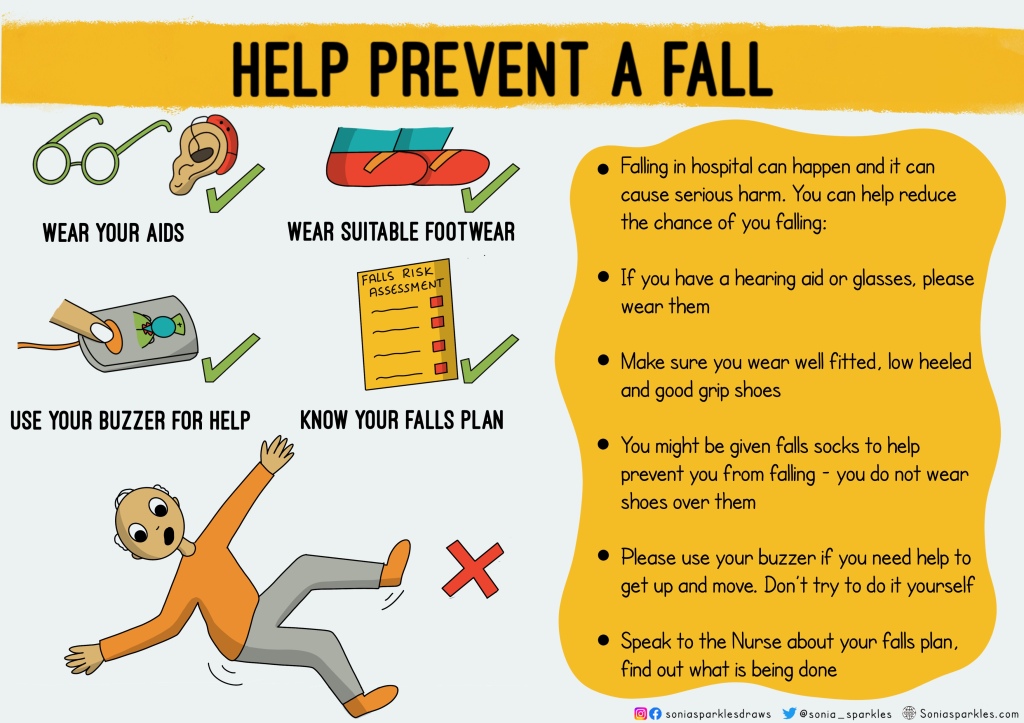
Falls. Do all patients know what to do to prevent a fall? Do they know an assessment is done? They don’t need an overly complicated separate leaflet, they just need to know what to do and what is done. Simple means more people will understand it.
Hand hygiene. We have reports, targets, audits and working groups for this; but again, do patients know what we are aiming for? Do they know when to challenges us and what hand hygiene means? After all it’s for them we do it. Encouraging them to ask and to be aware of when we should wash our hands could help stop the spread of germs.
Estimated date of discharge (EDD). It is important to have a date to go home in mind even though it might change so that patients have some understanding of how long they might be in hospital. Do patients know what it is? Do they know we are meant to set it for everyone? It needs to be more meaningful for patients (not just for hospital flow) as it can be frustrating not knowing how long you will be in hospital. Many times, patients might ask “when am I likely to go home” and be told “don’t know.” Now, with information like this, they can use it to challenge back and ask for their EDD

Hydration. Many patients don’t know what drinks are on offer or how important it is to keep hydrated. They might find a Nurse is encouraging them to keep drinking- but why? Do patients know why it is important? Do they know what to look out for regarding dehydration? It’s not just the job of Nurses to ensure all patients are hydrated, empower patients to do this themselves too! Encourage them
Morning ward round. These can seem scary to patients with lots of professionals assessing them. They might not feel confident asking for things to be explained or even know what a care plan is. We need to make them feel in charge, inquisitive and comfortable with what’s going on
Medication. Explain it in simple terms so patients know exactly what it does. They need to be aware of side effects. They need to be aware of how it helps them. They also need to be aware if they are in pain, they don’t need to suffer silently. Encourage them to ask for help if needed
Clean mouth. Often, patients might not think brushing their teeth is significant- informing them why it is can encourage them to do it more often. They don’t need to be embarrassed if they don’t have a toothbrush or need help with brushing their teeth, they need to know they can ask us.

Handover. How many times do we get something wrong on handover or miss something important? By involving the patient, less mistakes will happen, after all, it’s all about them! Bedside handover should be done more often. They help inform the patient of what is happening as well as allow them to include their needs

Visiting. Patients can feel really anxious, lonely or sad during hospital stays. It’s important they know what the rules are about visiting. It’s also important they know carers can come help them at anytime. This can be crucial to their well-being, recovery and advocacy.

Sitting out to eat. Such a simple one but many patients continue to lay down in bed to eat because they don’t know the benefits. Encouraging them to sit out does more than help their digestion, it gets them moving and active. Laying down all day isn’t good for them
Your poo matters. Yes I used the word poo. Everyone knows what it means. It makes patients feel less embarrassed & more confident in speaking about it. They need to know they are not bothering us by asking for help. Also, many falls happen when they don’t ask for help going to toilet
Understanding your care plan. I cannot emphasise enough how much we need to explain things. This helps them to know what to look out for, when somethings not right and if they need to speak up. They are our alert system, we need to use them more by educating them

Pressure ulcers. We have quality improvement projects on this, but how many include empowering patients to look out for them? Patient’s know their own body; ask them to raise concerns if they think they have a pressure ulcers. How many serious incidents could this reduce?

Getting dressed (EndPJParalysis) Just some gentle encouragement to get dressed and get moving. Mental health, well-being and motivation to get better can help patients during a challenging time in their life. Something as simple as getting dressed can help them transition from hospital to home

Blood clots. Life threatening and increased risk during hospital stay. Educating patients on what to look out for and what to do to reduce the risk of getting one is so important
Readiness to go home. Some simple things we can get patients to think about that can help with their discharge and get them safely home.

Informed decision making. It can be scary as a patient to ask why certain decisions are made. Sometimes it can be easy as a professional to not always ACTIVELY include the patient due to time constraints or pressures. Knowledge is power and comfort all patients need

Meal times. Sometimes, patients can be hungry between meals & not aware they can ask for food or might feel uncomfortable asking. Let them know it’s ok. Give help if needed. I’ll never forget a lady beside me on a ward who couldn’t reach her grapes -I helped feed them to her

And so with that, I hope my review of leaflets and attempt at creating empowering communication for patients has helped. Traditionally, many of the topics discussed above are spread out over several different leaflets, which can be information overload. Patients need something simple that they can refer to when needed. They won’t remember everything that is said to them, or everything that they read. Patient empowerment starts with meaningful communication
Thank you for taking the time to read! I have recently opened a shop and am still working through it’s set up – you can visit it via image below

Sonia Sparkles… this is truly patient centred care, free at the point of delivery and tuned to the anxiety and concerns of the hospital experiences. Thanks.
LikeLike